Just as technology has changed many aspects of our lives – from how we communicate to how we access information and even how we travel – it is also shaping the future of our health care. One area in which new and emerging technologies are making an impact is in the field of reconstructive surgery, a type of plastic surgery that involves restoring or reconstructing parts of the human anatomy that are damaged due to injury or congenital defect.
According to local surgeons, 3-D modeling and 3-D printing are greatly influencing the process of reconstructive surgeries and may even hold the key to medical advancements in the future.

3-D printing played a key role in the separation of conjoined twins Jadon and Anias McDonald, whose brains were fused together. The Children’s Hospital at Montefiore, New York, used 3-D printed models of the boys’ skulls and brains to plan the surgery, which was a success. (Photograph provided by The Children’s Hospital at Montefiore)
“3-D printing is a big area that’s emerging for plastic surgery,” Dr. Josh Waltzman, an independent plastic and reconstructive surgeon with a practice in Douglas Park, told the Business Journal. The technology is particularly useful for facial reconstruction, he said.
“What that involves is, say someone has a very traumatic accident, or it’s a child who has a congenital defect deformity that we’re going to reconstruct,” Waltzman said. “We can take a CT scan of that patient and upload that into software.” Through 3-D computer modeling using that imaging, doctors are able to create mock-ups of how to reconstruct bones based on the existing framework of a patient’s skull. This computer model can then be transferred to a 3-D printer, which is able to create anatomically accurate replicas for surgeons to practice on.
A recent, widely publicized application of this technology occurred in October, when surgeons at The Children’s Hospital at Montefiore in the Bronx separated two twins conjoined at the head. According to the hospital, twins Jadon and Anias McDonald had a complex case because their brains were fused.
Virtual planning technology was used to create 3-D computer models and 3-D printed replicas of the boys’ brains and skulls, which surgeons used to plan the separation surgery and the following reconstructive procedures on each boy. Although the two may require follow-up procedures, the separation surgery was a success. “This intricate procedure was greatly enhanced by cutting-edge 3-D technology that enabled the surgeons to see inside the boys’ brains,” Dr. Steven M. Safyer, president and CEO of the hospital, said in a press statement.

Dr. Josh Waltzman, who operates Waltzman Plastic & Reconstructive Surgery at Douglas Park in Long Beach, believes 3-D imaging and printing technologies will play an increasingly important role in medical advancements in his field. (Photograph by the Business Journal’s Larry Duncan)
One type of technology Waltzman is researching for potential use at his own practice is 3-D goggles. Existing technology allows doctors to take 3-D scans of patients from a tablet device, then augment them to show how a patient would look after a reconstructive or plastic surgery. Patients can then put on 3-D virtual reality goggles that project a 360-degree image of what they would look like from every angle, he explained.
3-D modeling has become crucial in reconstructive surgeries related to the body’s aorta, the largest blood vessel in the body, according to Kaiser Permanente’s Dr. Somjot Brar, who specializes in interventional cardiology.
“The aorta is the largest blood vessel in the body, and unlike the arteries in the heart that become narrowed and cause heart attacks, . . . sometimes it can balloon and become bigger than it should be,” Brar said. “We call that an aneurism. And when that happens, if it’s not repaired, the aorta can rupture. And the most common outcome if that happens is death.”
In this context, reconstructive surgery is employed using special tools to reinforce and repair the aorta. “That’s a really complicated area to work in, and the surgical options are very limited for some patients,” Brar said. The aorta is shaped like a question mark, with one end located next to the spine and the other right behind the breastbone.
In addition to this being a difficult location to operate, the shape of the aorta itself also varies from person to person, Brar said. Blood vessels connecting to the aorta are also a factor in surgery, which typically involves inserting a specially shaped stent with holes that must align with the blood vessels, he explained.
3-D modeling has helped tackle these complicating factors. “All of our patients will undergo a CT. And then that CT data is used to create the three-dimensional models of the patient’s anatomy on the computer,” Brar said. “So one can do kind of a virtual procedure of sorts using the patient’s exact anatomy.”
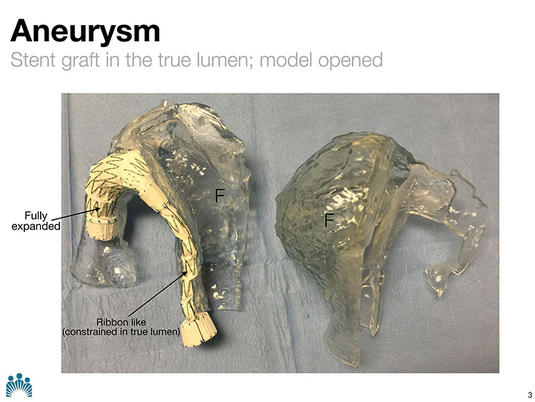
A 3-D printed model enables surgeons to practice inserting specially fitted stents into the aorta, the largest blood vessel in the body. According to Kaiser Permanente’s Dr. Somjot Brar, surgeons only get one chance to insert the stent so that it correctly aligns with a patient’s aorta and connected blood vessels. (Image courtesy of Kaiser Permanente)
For patients with particularly complex anatomies or other health care issues, these 3-D models are used to create printed replicas of their aortas for surgeons to practice on. “They allow us to be able to implant the devices to be able to see how the device is going to perform with that patient’s specific complicated and unique characteristics of their aortic anatomy,” Brar said.
While surgeons have been using computer-generated 3-D modeling for about four years, the use of 3-D printed anatomical replicas to plan surgical procedures has only been in practice for about a year and a half, Brar estimated. “I feel pretty strongly that some of these cases that we’ve done, I think, in large part they were successful because of the 3-D technology, including the printing,” he noted.
Beyond helping surgeons plan complex procedures, 3-D printing may hold the key to helping people regenerate their own tissues. A recently published study in the academic journal, Science Translational Magazine, detailed the findings of a group of researchers at Northwestern University who have developed a material called hyper-elastic bone using 3-D printing.
The newly created material is made from mineral components of bone and can be quickly produced with a 3-D printer, according to the study. The material is highly elastic and absorbent, and when implanted in a mouse, a rat and a primate, the bone “quickly integrated with surrounding tissues, and rapidly ossified and supported new bone growth without the need for added biological factors.” The research team that developed the material is hoping for human trials in the future.
“Eventually it would be great to say, if someone has lost an ear or a nose, can we just grow that off a scaffolding,” Waltzman said. “That’s kind of the next frontier.”
Other technologies beyond 3-D modeling and printing are influencing the future of reconstructive surgery. One area of advancement in technological testing and research is related to reconstructive surgery for breast cancer survivors, according to Waltzman.
“Emerging technologies in breast reconstruction have to do with the tissue expansion portion,” Waltzman said. “Oftentimes after a mastectomy, you don’t have enough skin to actually reconstruct [the breasts]. So you have to expand the skin with a tissue expander before you can actually put an implant in if you are doing that type of reconstruction,” he explained.

Palo Alto-based firm AirXpanders has developed a remote controlled medical device called AeroForm which allows women who have undergone mastectomies to expand their chest skin in preparation for breast reconstructive surgery without any injections. It is currently undergoing clinical trials. (Image courtesy of AirXpanders)
“Right now, patients have to come into our office every week, and they get filled up either with air or with saline injected into the expander to increase the size of it,” Waltzman continued. “But in the future, I think there will be expanders doing what is called auto-expansion, where the patient doesn’t have to come as frequently to the office for expansions, and it’s just a gradual process.”
A Palo Alto-based firm called AirXpanders Inc. has already developed such a product, which is currently undergoing clinical trials. AirXpanders has created a wireless tissue expander called AeroForm that is implanted within a patient’s chest. A remote control allows the patient to inflate the implant with small doses of carbon dioxide released from a device within the expander.
Dr. Kamakshi Zeidler, a San Jose-based plastic surgeon specializing in reconstructive and cosmetic breast surgeries, has patients participating in the national clinical trial for AeroForm and is looking forward to its FDA approval, which she said is likely imminent. The medical device, she noted, is already approved in Australia.
“It’s completely transformed their experience,” Zeidler said of her patients. “What the average patient goes through with the traditional expander with saline, they have to make appointments at the office for a procedure. . . . This appointment includes making the skin really clean and poking with a needle and injecting sterile saline,” she explained.
Zeidler reflected, “You know, it’s a little poke, just like getting your blood drawn. But you can imagine if you get your blood drawn every week for several weeks to a month, it all adds up in this whole process of everything else women go through. And as someone who watches women’s faces and sees them wince with a little pinch – I think one day we’ll look back and say this is pretty barbaric.”
Now, however, the new AeroForm device allows women to keep their clothes on and self-dose at home without an injection procedure. “It’s incredible, and the patients have said that,” Zeidler said. “They’ve loved how easy it is and how much they are a little bit in control of the process.”
In addition to making patients more comfortable, the device has also proven to speed up the skin expansion process, reducing the time between the expander insertion procedure and the final implant procedure by about half, Zeidler said.
